Introduction
Inflammation, a fundamental biological response to harmful stimuli, is an essential mechanism for the maintenance and repair of tissues. This process, characterized by five cardinal signs - rubor (redness), tumor (swelling), calor (heat), dolor (pain), and functio laesa (loss of function) - can be both beneficial and detrimental to the body. The understanding of inflammation's intricacies is crucial in various fields, including immunology, pathology, pharmacology, and medicine, as it provides insights into disease etiologies and potential therapeutic strategies. This course aims to provide a comprehensive overview of inflammation, its cellular and molecular mechanisms, and its role in health and disease.
Historical Perspectives
Inflammation has been observed since antiquity, with descriptions found in ancient Greek and Roman texts. However, it was not until the 17th century that Thomas Sydenham first coined the term "inflammation." The scientific understanding of inflammation evolved significantly over the subsequent centuries, culminating in the identification of cellular and molecular mediators during the 20th century.
Inflammatory Response: Definition and Characteristics
Definition
Inflammation refers to a localized protective response to tissue injury or infection, characterized by the activation of immune cells, the release of signaling molecules, and the subsequent recruitment and activation of additional immune cells.
Characteristics
Vascular Changes
The vascular changes that occur during inflammation involve vasodilation (increased blood flow) and increased vascular permeability, leading to extravasation of fluid, plasma proteins, and leukocytes from the bloodstream into the affected tissue.
Leukocyte Recruitment and Activation
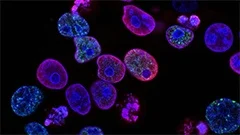
The recruitment and activation of leukocytes (white blood cells) is a critical component of inflammation, with neutrophils and macrophages being among the first cells to arrive at the site of injury or infection. These cells engulf and destroy pathogens, debris, and damaged tissue through phagocytosis.
Production of Signaling Molecules
The production and release of various signaling molecules, such as cytokines, chemokines, and prostaglandins, play a crucial role in the regulation of inflammation by modulating cellular activities, attracting immune cells, and mediating pain.
Classification of Inflammation
Inflammation can be classified based on its duration, intensity, and etiology:
- Acute Inflammation: A rapid and intense response to tissue injury or infection, lasting for a few days to several weeks. Acute inflammation is characterized by the release of pro-inflammatory cytokines, the recruitment of neutrophils, and the formation of pus.
- Chronic Inflammation: A long-lasting response to persistent tissue injury or infection, lasting for several weeks to years. Chronic inflammation is characterized by the infiltration of immune cells (e.g., macrophages, lymphocytes), the production of fibrous tissue, and the potential development of pathological conditions, such as atherosclerosis and cancer.
- Inflammatory Response to Sterile Injury: Inflammation can occur in the absence of microbial infection, as seen in ischemia-reperfusion injury, tissue trauma, or autoimmune diseases. The immune response in these cases is primarily mediated by damage-associated molecular patterns (DAMPs) and pattern recognition receptors (PRRs).
Key Cellular and Molecular Players in Inflammation
Leukocytes
Neutrophils, macrophages, dendritic cells, and lymphocytes are among the key leukocytes involved in inflammation. These cells exhibit diverse functions, including phagocytosis, antigen presentation, cytokine production, and regulation of the immune response.
Neutrophils
Neutrophils are the most abundant leukocytes in circulation and play a crucial role in acute inflammation by engulfing and destroying pathogens through phagocytosis. They are recruited to sites of infection or tissue injury via chemokines and adhesion molecules.
Macrophages
Macrophages are versatile immune cells that play essential roles in both acute and chronic inflammation. They can phagocytose pathogens, debris, and damaged tissue, as well as produce cytokines and chemokines to modulate the immune response. Macrophages also play a critical role in wound healing and tissue repair by promoting angiogenesis, fibroblast activation, and extracellular matrix deposition.
Dendritic Cells
Dendritic cells are antigen-presenting cells that play a pivotal role in the adaptive immune response. They capture, process, and present antigens to T lymphocytes, thereby initiating adaptive immunity. During inflammation, dendritic cells can also produce pro-inflammatory cytokines and chemokines to orchestrate the immune response.
Lymphocytes
T lymphocytes and B lymphocytes are important components of the adaptive immune response during inflammation. T lymphocytes can differentiate into various effector cells (e.g., CD4+ T helper cells, CD8+ cytotoxic T cells) that exhibit cytotoxic or regulatory functions, respectively. B lymphocytes produce antibodies to neutralize pathogens and facilitate their elimination by phagocytic cells.
Cytokines and Chemokines
Cytokines and chemokines are signaling molecules that play essential roles in the regulation of inflammation. They act as intercellular messengers, modulating cellular activities, recruiting immune cells to sites of injury or infection, and mediating pain. Some key cytokines and chemokines involved in inflammation include:
Pro-inflammatory Cytokines
- Interleukin-1 (IL-1)
- Interleukin-6 (IL-6)
- Tumor Necrosis Factor-alpha (TNF-α)
- Interferon-gamma (IFN-γ)
Anti-inflammatory Cytokines
- Interleukin-4 (IL-4)
- Interleukin-10 (IL-10)
- Transforming Growth Factor-beta (TGF-β)
Coagulation and Fibrinolysis
Coagulation and fibrinolysis are closely intertwined processes that play essential roles in maintaining hemostasis during inflammation. Activated platelets, coagulation factors, and fibrinolytic enzymes regulate these processes to prevent excessive bleeding or clotting. Dysregulation of coagulation and fibrinolysis can lead to thrombosis or disseminated intravascular coagulation (DIC), which are associated with poor outcomes in various inflammatory conditions.
Therapeutic Strategies for Modulating Inflammation
Several therapeutic strategies have been developed to modulate inflammation, including:
- Non-steroidal Anti-inflammatory Drugs (NSAIDs): NSAIDs inhibit the activity of cyclooxygenase enzymes (COX-1 and COX-2), thereby reducing the production of pro-inflammatory prostaglandins and leukotrienes. Commonly used NSAIDs include ibuprofen, naproxen, and aspirin.
- Corticosteroids: Corticosteroids (e.g., prednisone, dexamethasone) inhibit the production of pro-inflammatory cytokines and chemokines, as well as modulate the activity of immune cells. They are often used to treat acute and chronic inflammation.
- Biologic Therapies: Biologic therapies target specific molecules involved in inflammation, such as pro-inflammatory cytokines (e.g., TNF-α), integrins, and adhesion molecules. Examples of biologic therapies include tumor necrosis factor alpha inhibitors (e.g., infliximab, etanercept) and integrin antagonists (e.g., natalizumab).
- Janus Kinase (JAK) Inhibitors: JAK inhibitors block the signaling pathways of cytokine receptors, thereby reducing the production of pro-inflammatory cytokines and modulating immune cell activity. Examples of JAK inhibitors include tofacitinib and baricitinib.
- Targeting the Complement System: The complement system plays essential roles in inflammation by mediating the destruction of pathogens and the recruitment of immune cells. Targeting components of the complement system (e.g., C5) with monoclonal antibodies has shown promise in the treatment of autoimmune diseases.
Conclusion
Inflammation is a complex and multifaceted process that plays crucial roles in the maintenance of tissue homeostasis, as well as the pathogenesis of various diseases. The intricate interplay between cellular players, cytokines, and signaling pathways makes inflammation an attractive therapeutic target for drug development. A better understanding of the molecular mechanisms underlying inflammation will undoubtedly lead to the development of more effective and targeted therapies for a wide range of clinical conditions.
MCQ: Test your knowledge!
Do you think you know everything about this course? Don't fall into the traps, train with MCQs! eBiologie has hundreds of questions to help you master this subject.
These courses might interest you
Create a free account to receive courses, MCQs, and advice to succeed in your studies!
eBiologie offers several eBooks containing MCQ series (5 booklets available free for each subscriber).